Medically Reviewed by:Scientific Advisory Board
Navigating the unchartered waters of diabetes insipidus is a challenging journey. To overcome it, knowledge and understanding become your compass to lead you through excessive urination and extreme thirst. This blog post serves as your guide that provides an in-depth insight into this condition while giving you the confidence to face whatever comes ahead on this voyage with courage and optimism.

Short Summary
-
Diabetes Insipidus is a condition affecting the body’s ability to retain water and regulate fluid balance.
-
Diagnosis involves physical examination, review of medical history, and tests such as the water deprivation test.
-
Treatment options include medications like desmopressin along with lifestyle changes, low-salt/low protein diet & healthy food choices for better symptom management..
Diabetes Insipidus Explained

Your body is like a city, where hormones are its traffic lights. In the case of diabetes insipidus (marked by an excessive output of pale urine and water retention difficulties), it’s as though these signals have malfunctioned. This disorder should not be confused with diabetes mellitus, another condition that can bring on similar outcomes in terms of fluid production. Both cities require different solutions for their transportation problems, yet they still remain distinct from one another. New York compared to Paris being just such an example!
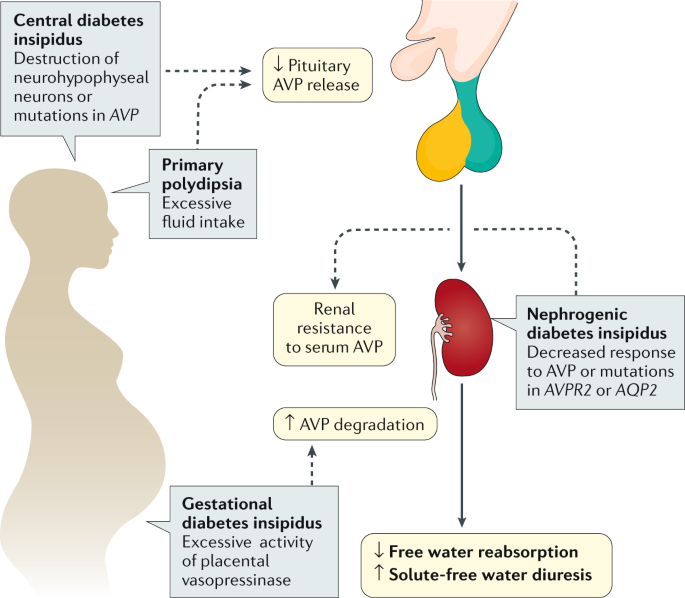
The antidiuretic hormone (ADH), created by the hypothalamus and stored inside the pituitary gland, works relentlessly behind the scenes to stabilize your bodily fluids through managing this traffic. Yet when there’s disruption within either ADH formation or discharge, four kinds of insulin insipidus arise: central, nephrogenic dipsogenic & gestational forms respectively.
Regrettably, no cure exists for this health issue, but most affected individuals are able to live otherwise typical lives as long as comprehension levels reach satisfactory heights surrounding all types of Insulin Insipidus plus how each might affect them differently personally speaking anyway.
Central Diabetes Insipidus
Central diabetes insipidus is comparable to a citywide power outage – caused by an issue in either the hypothalamus or pituitary gland, which ultimately leads to too little vasopressin. Much like when lights are out during a blackout, this condition can come on suddenly due to damage of these glands. The result? Excessive urine produced since the kidneys cannot retain fluids properly, just as if all our water was being thrown away because traffic signals were not working correctly. In other words, central diabetes causes significant disruption akin to that found in everyday life after such sudden and unpredictable events.
Nephrogenic Diabetes Insipidus
In a city with congenital nephrogenic diabetes insipidus, the traffic lights are operational but they are being disregarded by drivers, the kidneys. This health issue is caused due to lack of response of kidney towards vasopressin, leading to stagnation and congestion in fluids within the body similar to motorists going on strike causing immense inconveniences.
Genetic mutations, usage of certain medications, and electrolyte imbalances might be at its origin which lead into inability for concentrating urine & controlling water balance. Culminating as multiple digestive/kidney diseases like drought-like state if it were happening in an urban area affected from this problem between officers and workers’ dispute impacting majorly amongst the public therewith.
Dipsogenic Diabetes Insipidus
In Dipsogenic Diabetes Insipidus, the hypothalamus is at fault for excessive drinking and an unquenchable thirst. It’s like a city with no water fountains that never quiets its citizens’ dryness. There’s trouble treating this condition effectively as it isn’t related to ADH production – there’s no way of negotiating or fixing traffic lights here. All we can do is try our best to ease their endless parched mouths. That’s why researchers on dipsogenic diabetes insipidus are always looking for new solutions so they may have some success in helping those affected by the disorder finally find relief from their endless thirst.
Gestational Diabetes Insipidus
Gestational diabetes insipidus is an uncommon situation that occurs unexpectedly during pregnancy. It’s triggered by the production of too much enzyme from the placenta which destroys antidiuretic hormone (ADH). This condition can be compared to a city appearing out of nowhere with lights being taken down all around it. Fortunately, gestational diabetes passes after childbirth – almost as though this new “city” just vanished into thin air without any warning!
Symptoms and Warning Signs
The signs of diabetes insipidus are similar to a city stuck in gridlock: profuse urination and dehydration. It is very important that the warning signals do not go ignored, just as responding quickly can help manage traffic issues effectively. As soon as one notices these symptoms - much like hitting an emergency button for assistance with too many cars on the road - medical aid should be sought without delay so potential problems related to severe water loss may be avoided.
Diagnosis Process
In order to diagnose diabetes insipidus, it is necessary to undergo a physical exam and review the patient’s medical history. To other tests. The water deprivation test has been shown as an accurate indicator for determining whether or not this condition exists, just like cutting off water supply from the city would show how well its resources manage with less fluid. During this assessment, no liquid should be consumed by the individual being tested. If excessive amounts of dilute urine are produced despite these restrictions, then diabetes insipidus can likely be diagnosed.
Treatment Options
Just like each city has its own unique approaches to handling traffic flow, the treatment for diabetes insipidus depends on what type it is. Common treatments are medication such as desmopressin and adapting one’s lifestyle habits. Desmopressin can be viewed similarly to a supervisor that maintains order over congestion when general streetlights don’t work. This works well in cases of central diabetes insipidus and gestational diabetes insulin resistance too.
There’s more than just reversing bad conditions or appointing someone new – managing all forms of diabetes requires certain changes in behavior as if citizens were trained better usage methods with water resources which helps avoid overpopulation/traffic issues within cities even Similarily enough - For both types involving central or gestational-linked diabetics.
Managing Diabetes Insipidus
Living with diabetes insipidus is like a journey through an area of variable and unpredictable traffic conditions. Controlling the intake of fluids, observing serum sodium levels and taking medication all play key roles in successful management.
Adopting a low-salt and protein eating plan can help ease symptoms. Just as when citizens utilise non-motorised transport such as buses or bikes to cut down on congestion. With the right strategies employed managing this condition becomes more straightforward.
Risk Factors and Prevention
There are certain factors that increase the risk of developing diabetes insipidus, such as having a family history of it or suffering from kidney disease. To this, certain medications like diuretics and brain surgery/head injury also up one’s chances of being affected by cranial diabetes insipidus, almost as if they were more vulnerable when caught in traffic.
Unfortunately, there is no known way to prevent or develop the condition. Seeking medical assistance right away should any symptoms arise can be hugely beneficial.
Complications and Prognosis
Much like any city dealing with traffic problems, if diabetes insipidus is not properly managed it can cause difficulties. Primarily this will be in the form of dehydration just as a town without water would suffer greatly. Fortunately, careful management usually results in successful outcomes, similar to when a metropolis finds solutions for alleviating congestion issues and guaranteeing access to vital resources such as H2O.
Specific people such as infants, seniors or those with mental health conditions are at greater risk from adverse consequences that may even include death due to Diabetes Insipidus. They must ensure extra precautionary steps are taken while traversing urban environments.
Clinical Trials and Research
As city planners tirelessly strive to improve traffic conditions, medical researchers are equally dedicated in their research of diabetes insipidus. Clinical trials and scientific studies have acted as guideposts that help identify new measures for prevention, recognition or control of the disease, which improves people’s quality of life.
To obtain information about advances related to this disorder, you can find out more on www.ClinicalTrials.gov. Similar to finding accurate updated traffic news helps commuters find better ways around town efficiently.
Diet and Nutrition Impact
Adopting a nutritional regime similar to redesigning roads and revising traffic rules can help reduce diabetes insipidus symptoms. Incorporating low-salt, low protein foods into the diet is like improving city infrastructure for smoother movement of vehicles on its roadways. Adding plenty of watery fruits and vegetables is similar to encouraging citizens to cycle or use public transport. With such dietary adjustments in place, managing this condition will be less laborious than navigating a busy street during rush hour!
Summary
Exploring the terrain of diabetes insipidus can be daunting, but with suitable information and instruments it is quite conquerable. Being aware of all the different kinds of this condition, recognizing its signs, learning how to diagnose them, and having knowledge about available treatments, is like having a detailed guidebook for discovering this city.
It’s important not to forget that even though managing diabetes insipidus isn’t effortless (similar to going through congested traffic or limited access points in an actual urban area), by following up with proper plans, taking regular check-ups seriously and leading a balanced lifestyle you have high chances to move around without disruption.
Frequently Asked Questions
What does diabetes insipidus cause?
Diabetes insipidus can cause extreme thirst, frequent urination and severe dehydration if left untreated. It is unrelated to the more widespread diabetes mellitus but results in having to make excessive amounts of urine regularly.
What deficiency causes diabetes insipidus?
Diabetes insipidus occurs due to a deficiency in antidiuretic hormone (ADH), also referred to as vasopressin, which helps maintain hydration by letting the kidneys conserve water. The hypothalamus region of the brain produces ADH. Thus, without sufficient production of this substance, it can result in dehydration and eventually diabetes insipidus.
What is the difference between diabetes insipidus and diabetes mellitus?
Diabetes mellitus and diabetes insipidus are distinct conditions: the former is a metabolic disorder caused by insufficient insulin production, while the latter results in excessive urine output and water loss.
What are the symptoms of diabetes insipidus?
Diabetes insipidus is a medical condition in which the production of pale urine and excessive urination leads to dehydration. This disorder occurs due to an inadequate amount of antidiuretic hormone, responsible for maintaining water balance within the body. Without this vital chemical compound, it becomes difficult for one’s system to store enough water, leading them into experiencing very severe levels of thirst or dryness associated with such scenario as mentioned before.
How is diabetes insipidus diagnosed?
During a physical exam, medical history is taken into account and sometimes a water deprivation test may be used to diagnose diabetes insipidus.
References, Studies and Sources:
https://www.niddk.nih.gov/health-information/kidney-disease/diabetes-insipidus/
More About Circufiber.com and Healthcare disclaimer:
Always consult your physician before beginning any program. This general information is not intended to diagnose any medical condition or to replace your healthcare professional. If you experience any pain or difficulty, stop and consult your healthcare provider. Circufiber.com socks are clinically proven to improve micro-circulation in feet and lower extremities in people with Diabetes.
More Author Information:
Dr. Capozzi is a board-certified foot surgeon through the American Board of Foot and Ankle Surgery. He is a Diplomate of the American Academy of Wound Management and Fellow of the American College of Foot and Ankle Surgeons. He completed a three-year residency program in Foot and Ankle Reconstructive Surgery at St. Francis Hospital & Medical Center in Hartford, CT in 2010. Dr. Capozzi is a board-certified Wound Specialist® granted by the American Academy of Wound Management. He is also board-certified in Foot Surgery through the American Board of Foot and Ankle Surgery.




