Medically Reviewed by:Scientific Advisory Board
It's not uncommon for people with diabetes to experience a range of foot-related issues. Yellowing of the bottom of the feet can be a cause for concern, as it often signals underlying health problems. In this article, we'll delve into the possible reasons behind this symptom and how to address it effectively.

One of the chief causes of yellowing feet in diabetics is a condition called diabetic neuropathy. This nerve damage primarily affects the extremities and can lead to changes in skin color, such as yellowing, due to limited blood flow and nerve function.
Another possible culprit behind yellowing feet could be a fungal infection, especially if there's also an unpleasant odor or itchy sensation. Athlete's foot, for example, is quite common among diabetic individuals and may cause a yellowish tint to the skin on the bottom of the feet. Identifying and treating the root cause of this discoloration is essential to properly manage diabetes and maintain overall foot health.
Understanding Diabetes and Yellow Feet
We'll begin by discussing how diabetes affects the feet, and, specifically, the reasons behind the yellowing of their soles. To fully comprehend this phenomenon, it's crucial to recognize the vital role our feet play in our daily activities. However, sometimes complications arise, and many people with diabetes can experience foot-related issues, one of which includes yellowing.
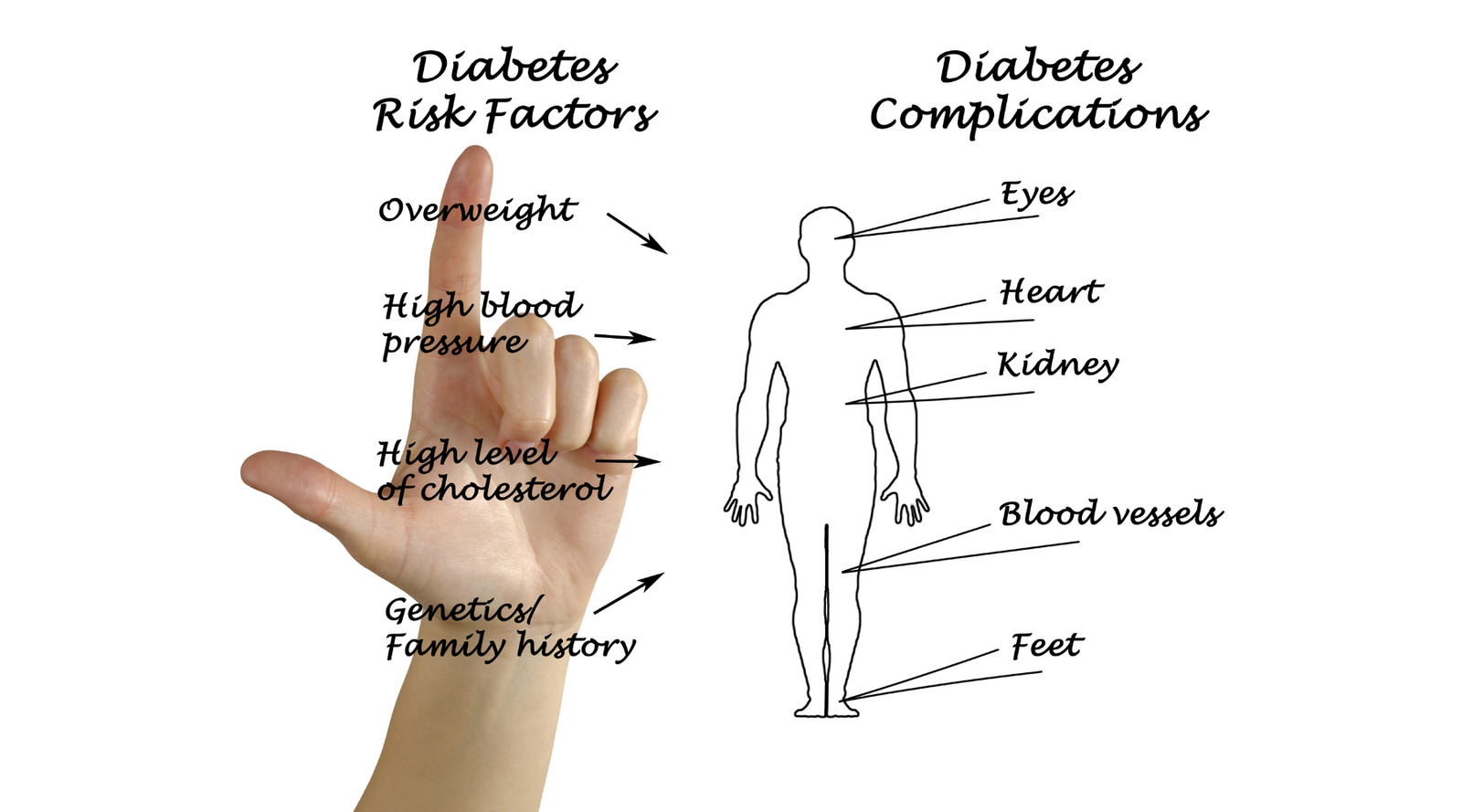
Diabetes and its complications have a notable impact on the health of our feet. Both type 1 and type 2 diabetes can lead to peripheral neuropathy, resulting in decreased sensation in the feet. This condition increases the likelihood of injuries, infections, and skin breakdown. Moreover, diabetes often impairs blood circulation, causing further damage to our feet by delaying the healing process.
Against this backdrop, we can identify the main factors contributing to yellow feet:
-
Tinea pedis: Also known as athlete's foot, this fungal infection can be more prevalent in people with diabetes due to a weakened immune system and poor circulation. Tinea pedis causes dry, flaky skin and can lead to yellowing of the soles.
-
Calluses and corns: These are thickened layers of skin that form due to consistent pressure or friction on specific areas of the feet. Calluses tend to develop on the soles, while corns frequently appear on the toes. In individuals with diabetes, changes in foot structure may lead to excessive pressure on certain parts of their feet, resulting in the formation of calluses and corns, which can be yellowish in color.
-
Poor circulation: Diabetic peripheral arterial disease (PAD) can restrict blood flow in the feet, depriving them of the nutrients and oxygen they need. As a result, skin becomes discolored, often appearing yellow or reddish.
Taking control of blood sugar levels will positively impact the health of our feet. Besides, we can adopt the following practices to minimize the risk of complications:
- Inspect feet daily: Look for any cuts, blisters, redness, or swelling. Don't forget to check between the toes.
- Keep feet clean and dry: Wash feet daily, and dry them thoroughly to prevent fungal infections.
- Choose the right shoes: Wear comfortable, well-fitted shoes that provide adequate support and don't cause excessive pressure.
- Use diabetic socks: Choose socks that are seamless, moisture-wicking, and specifically designed for individuals with diabetes, like those from Circufiber.com. These provide extra cushioning and reduce the risk of injuries or infections.
By understanding the connection between diabetes and yellow feet, we empower ourselves to take the necessary steps to prevent complications and maintain the overall health of our feet.
Common Causes of Yellowing in Diabetic Feet
Diabetic feet can experience a variety of issues, and yellowing is one of the more common symptoms. There are several explanations for this discoloration, and in this section, we will discuss some of the most likely causes.
Infection: The presence of an infection is often the primary cause of yellowing feet in those with diabetes. Individuals with diabetes frequently suffer from reduced blood circulation, which can delay the healing of cuts or sores. This slow healing can make wounds more susceptible to infection. Signs of infection might include swelling, redness, warmth, or a yellow discharge. If you notice these indications, it's vital to seek medical attention right away.
Tinea pedis: Also known as athlete's foot, tinea pedis is a common fungal infection affecting the skin of the feet. People with diabetes are at a higher risk of developing this infection due to compromised immune systems and reduced blood circulation. Tinea pedis tends to cause yellowing around the soles of the feet, on the sides, and between the toes. Over-the-counter antifungal creams can often clear up the infection, but consult a healthcare professional if symptoms persist.
Calluses and corns: In people with diabetes, the development of calluses and corns can be particularly prevalent. This thickening of the skin may lead to yellowing, especially on the soles and sides of the feet. Proper foot care, including moisturizing and regular inspections, can help keep these issues at bay.
Nail fungus: Onychomycosis, a fungal nail infection, is more likely to affect people with diabetes. This type of infection leads to toenails becoming thick, brittle, and yellow. Treatment may include oral antifungal medications, topical treatments, or, in severe cases, the removal of the affected nail.
If you're experiencing yellowing of your feet, it's essential to see a healthcare professional for appropriate diagnosis and treatment.
Prevention and Treatment Strategies
Realizing the importance of foot care for diabetics, we've put together a list of prevention and treatment strategies to help keep your feet healthy.
Proper self-care can minimize the risk of complications from diabetes, including yellowing skin at the bottom of your feet.
- Routine foot inspections: Examine your feet daily, paying attention to any changes in color, texture, or sensation. If you notice a yellowish hue on the soles of your feet, consult your healthcare provider to identify the cause and find appropriate treatment.
- Keep your feet clean: Maintain good foot hygiene by washing your feet daily with mild soap and warm water. Make sure to dry your feet thoroughly, especially between the toes, as moisture retention could lead to fungal infections and discoloration.
- Proper footwear: Invest in quality, well-fitted shoes and socks designed for people with diabetes. Products like those offered by Circufiber.com have been medically proven to help diabetics protect their feet. Avoid tight, ill-fitting shoes and socks, as they could provoke skin problems and limit blood flow.
- Trim your nails correctly: To prevent ingrown toenails and infections, make sure to trim your nails straight across and gently file any sharp edges.
- Moisturize: Apply moisturizing lotion to your feet daily, except between your toes, to maintain healthy skin and minimize the risk of yellowing or cracking skin.
Apart from foot care, pursuing optimal diabetes management is crucial to prevent diabetic foot complications.
Strategies include:
- Blood sugar control: Keeping blood glucose levels in check is essential to reduce the risks associated with diabetes, including yellowing skin. Regular monitoring of blood sugar levels can help spot any discrepancies and enable prompt action.
- Proper diet: Maintain a well-balanced diet, low in saturated fats, sodium, and simple sugars. Emphasizing whole grains, lean meats, and fresh fruits and vegetables can provide your body with the nutrients it needs.
- Staying active: Engaging in regular exercise not only contributes to maintaining a healthy weight, but it also improves blood circulation, which is necessary for preventing diabetes-related foot issues.
- Regular check-ups: Schedule routine medical appointments, so your healthcare provider can monitor your overall health and identify any diabetes-related complications early.
Being proactive about foot care and adopting these prevention and treatment strategies can significantly reduce the risk of diabetic foot complications, including the yellowing skin at the bottom of your feet.
Learn More About The Two Weeks to Better Feet Circufiber Challenge 👇
Conclusion
We've explored the causes and implications of yellowing at the bottom of feet in people with diabetes. As previously discussed, this discoloration can be attributed to:
- Altered skin pigmentation
- Tinea infections
- Diabetic neuropathy
- Calluses and poor circulation
To tackle these concerns, it's crucial for diabetics to monitor their foot health, maintain proper hygiene, and consult a doctor when necessary. We strongly encourage the following practices:
- Regularly inspecting feet for any changes
- Keeping feet clean and moisturized
- Wearing comfortable and protective footwear, such as specially designed diabetic socks from Circufiber.com
- Consulting a podiatrist for regular check-ups and to address any concerns
It's our belief that all diabetics deserve to have healthy, pain-free feet. By arming ourselves with accurate information and taking preventive measures, we can minimize complications and enjoy a better quality of life.
Remember, diligent foot care is paramount to ensuring one's well-being with diabetes, so it's essential to address any issues as soon as they arise.
References and Sources:
https://diabetes.org/diabetes/foot-complications
More About Circufiber.com and Healthcare disclaimer:
Always consult your physician before beginning any program. This general information is not intended to diagnose any medical condition or to replace your healthcare professional. If you experience any pain or difficulty, stop and consult your healthcare provider. Circufiber.com socks are clinically proven to improve micro-circulation in feet and lower extremities in people with Diabetes.
More Author Information:
Dr. Capozzi is a board-certified foot surgeon through the American Board of Foot and Ankle Surgery. He is a Diplomate of the American Academy of Wound Management and Fellow of the American College of Foot and Ankle Surgeons. He completed a three-year residency program in Foot and Ankle Reconstructive Surgery at St. Francis Hospital & Medical Center in Hartford, CT in 2010. Dr. Capozzi is a board-certified Wound Specialist® granted by the American Academy of Wound Management. He is also board-certified in Foot Surgery through the American Board of Foot and Ankle Surgery.