Medically Reviewed by:Scientific Advisory Board
Diabetes and metabolism are intimately entwined, each influencing the other in significant ways. We're here to shed light on this intricate relationship, providing you with the knowledge you need to manage your health effectively.
Metabolism is our body's process of converting food into energy needed for life's basic functions. When we talk about diabetes, we're specifically focused on how the body uses glucose or sugar, which is a critical source of fuel for our cells. In people without diabetes, insulin helps regulate this process smoothly. But for those living with diabetes, the story changes.
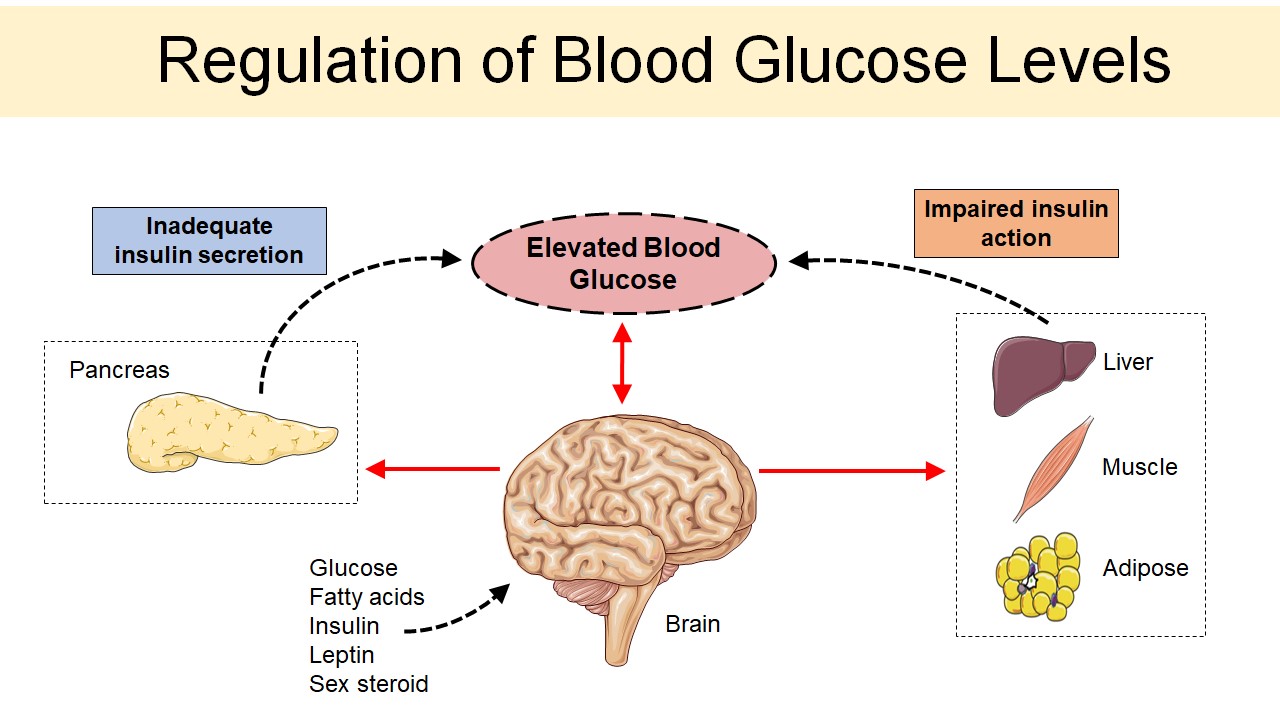
In cases of both Type 1 and Type 2 diabetes, there can be an imbalance in the way our bodies use glucose - leading to elevated blood sugar levels that carry serious health risks if not managed properly. It's crucial that we understand these dynamics so that we can take appropriate steps towards maintaining optimal health.
Understanding the Connection Between Diabetes and Metabolism
We'll start by defining what we mean when we refer to these two terms. Diabetes is a chronic health condition marked by high blood sugar levels, while metabolism refers to how your body uses food for energy.
When you have type 2 diabetes, your body either resists the effects of insulin — a hormone regulating the movement of sugar into cells — or doesn't produce enough insulin to maintain a normal glucose level. This can cause an accumulation of sugars in your bloodstream, hence high blood sugar levels.
Diabetes also affects how our bodies break down and use nutrients from food - a process known as metabolic function. In healthy individuals, carbohydrates from food are broken down into glucose in the digestive tract. This glucose then enters our bloodstream, causing blood glucose levels to rise.
Role of Insulin in Glucose Metabolism
Acting as the key to unlock our body's cells, insulin allows glucose to enter and be used for energy. Without this vital hormone, we'd have a buildup of blood sugar leading to hyperglycemia.
Let's break down how it all works:
- Once we eat food, our bodies break it down into various nutrients. Among these is glucose—a primary source of energy.
- As our blood glucose levels rise, the pancreas responds by releasing insulin.
- Like a diligent gatekeeper, insulin attaches to cells throughout our bodies. This attachment opens doors allowing glucose to enter the cells.
- Inside these cells, glucose is either used immediately for energy or stored for later use.
In individuals with diabetes however, this process doesn't function as it should. Their bodies either don't produce enough insulin or can't effectively use what they do produce—resulting in elevated blood sugar levels.
To illustrate this point visually:
| Condition | Blood Sugar Level | Insulin Response |
|---|---|---|
| Normal | Increases after eating | Adequate amount released; Glucose enters cells |
| Diabetes | Increases after eating | Inadequate amount released/Not properly utilized; Less/no entry of glucose into cells |
The understanding of this process underlines why managing insulin levels is crucial for people living with diabetes. It also sheds light on why maintaining a balanced diet and regular physical activity—both known influencers of insulin sensitivity—are often recommended lifestyle modifications for those diagnosed with diabetes.
In essence, when there's an imbalance between your body's demand for insulin and its ability to produce/use it effectively—the scales tip towards diabetes. That said, knowing how insulin functions can provide us insights on how best to manage and possibly prevent this chronic condition from developing.
Impact of Diabetes on Energy Production
We're about to dive into a topic that's crucial for understanding how our bodies function, particularly in relation to diabetes. It's all about the way energy is produced within us and how this process can be impacted by the presence of diabetes.
One key aspect of this is energy production, primarily achieved through metabolism - the process where our body converts what we eat and drink into usable energy. Now here’s where things get interesting for those with diabetes.
In a body functioning without diabetes, carbohydrates from food are broken down into glucose during digestion. This glucose moves into your bloodstream and insulin helps this glucose enter cells where it can be used for energy. But when you have diabetes—either Type 1 or Type 2—the process isn't so smooth.
Type 1 diabetics lack sufficient insulin due to an autoimmune response destroying insulin-producing cells in their pancreas. On the other hand, people with Type 2 diabetes do produce insulin but their cells become resistant to it over time.
- Type 1 Diabetes: The absence of enough insulin means glucose remains in the bloodstream rather than entering the cells.
- Type 2 Diabetes: Although there's ample insulin, resistance prevents effective use resulting in high blood sugar levels.
Here's a quick glance at how these two types affect overall energy production:
| Type | Insulin Presence | Use of Glucose |
|---|---|---|
| 1 | Low | Limited |
| 2 | High | Inefficient |
When either scenario occurs, your body gets starved of its primary source of fuel despite having high levels of glucose in your bloodstream which leads to feeling lethargic or fatigued—a common symptom among individuals living with diabetes.
This disruption also triggers a cascade effect on other metabolic pathways as the body scrambles for an alternative energy source. It's like a domino effect, one part of the system gets knocked off balance and it starts impacting other areas too.
In the case of prolonged high blood sugar levels, your body starts to break down fat for energy—a process called ketosis. While this might sound appealing to those wanting to lose weight, if left unchecked, ketosis can lead to a dangerous condition called ketoacidosis which is potentially life-threatening.
Managing Diabetes Through Metabolic Control
We're delving into the exciting science of metabolism in our quest to understand and manage diabetes better. Isn't it fascinating how our bodies convert what we eat into energy? This process, known as metabolism, plays a crucial role in managing diabetes.
Our bodies break down carbohydrates from food into glucose, which is then released into the bloodstream. In response to this surge in blood sugar levels, our body releases insulin – an essential hormone that helps cells absorb glucose for energy or storage. However, when you have diabetes, your body either doesn't produce enough insulin or can't use it effectively. That's where metabolic control comes in.
Controlling your body's metabolism essentially means regulating these processes to maintain stable blood sugar levels. Here are some ways you could achieve this:
- Regular physical activity: Exercise increases insulin sensitivity and helps your muscles use up more glucose.
- Healthy diet: Choosing foods low on the glycemic index (GI) can reduce spikes in blood sugar levels after meals.
- Medication: Some drugs help decrease the amount of glucose absorbed from food or increase its usage by cells.
In closing, controlling metabolism proves to be an effective approach toward managing diabetes. It's not just about taking medication; it also involves lifestyle changes like diet and exercise. With hope and determination, we believe everyone living with this condition can lead healthier lives.
Conclusion: The Interplay Between Diabetes and Metabolism
We've journeyed quite a bit into the complex relationship between diabetes and metabolism. Our understanding is more profound now, knowing that these two are not separate entities but closely intertwined aspects of our body's functioning.
Diabetes, primarily characterized by higher levels of blood sugar, is often influenced by metabolic disorders. This means if you're dealing with diabetes, your metabolism isn't working as smoothly as it should. It’s the inefficient utilization or production of insulin that leads to metabolic disturbances creating a cycle where one aggravates the other.
However, we shouldn't forget that this interplay can be managed effectively with proper self-care strategies:
- Regular exercise helps in maintaining healthy body weight and improves insulin sensitivity.
- Balanced nutrition plays a crucial role in managing blood sugar levels and overall metabolic health.
- Adequate sleep regulates important hormones affecting both glucose metabolism and appetite.
- Stress management assists in controlling hormonal fluctuations that could interfere with glucose metabolism.
Understanding how diabetes affects your metabolism offers an advantage. You'll be better equipped to manage your condition proactively rather than reactively. Remember - knowledge is power when it comes to managing chronic conditions like diabetes.
References, Studies and Sources:
https://www.medicalnewstoday.com/articles/diabetes-and-metabolism
More About Circufiber.com and Healthcare disclaimer:
Always consult your physician before beginning any program. This general information is not intended to diagnose any medical condition or to replace your healthcare professional. If you experience any pain or difficulty, stop and consult your healthcare provider. Circufiber.com socks are clinically proven to improve micro-circulation in feet and lower extremities in people with Diabetes.
More Author Information:
Dr. Capozzi is a board-certified foot surgeon through the American Board of Foot and Ankle Surgery. He is a Diplomate of the American Academy of Wound Management and Fellow of the American College of Foot and Ankle Surgeons. He completed a three-year residency program in Foot and Ankle Reconstructive Surgery at St. Francis Hospital & Medical Center in Hartford, CT in 2010. Dr. Capozzi is a board-certified Wound Specialist® granted by the American Academy of Wound Management. He is also board-certified in Foot Surgery through the American Board of Foot and Ankle Surgery.